Kirkby New Model General Practice
Executive Summary
This paper draws on the work carried out by Local Care Direct and Turning Point (LCD/TP) in developing their approach to services in General Practice. In addition other components are drawn from models of care in operation elsewhere in the UK or USA and gathered by the author.
This paper outlines the model, its potential implementation pathway and seeks to demonstrate the cost neutral approach required to be sustainable in current economic times.
Model Components
The cycle of general practice; Access, Intervention and Follow Up, form the building blocks of the model. For convenience each of these components will be considered in turn before assembling the overall model
Access
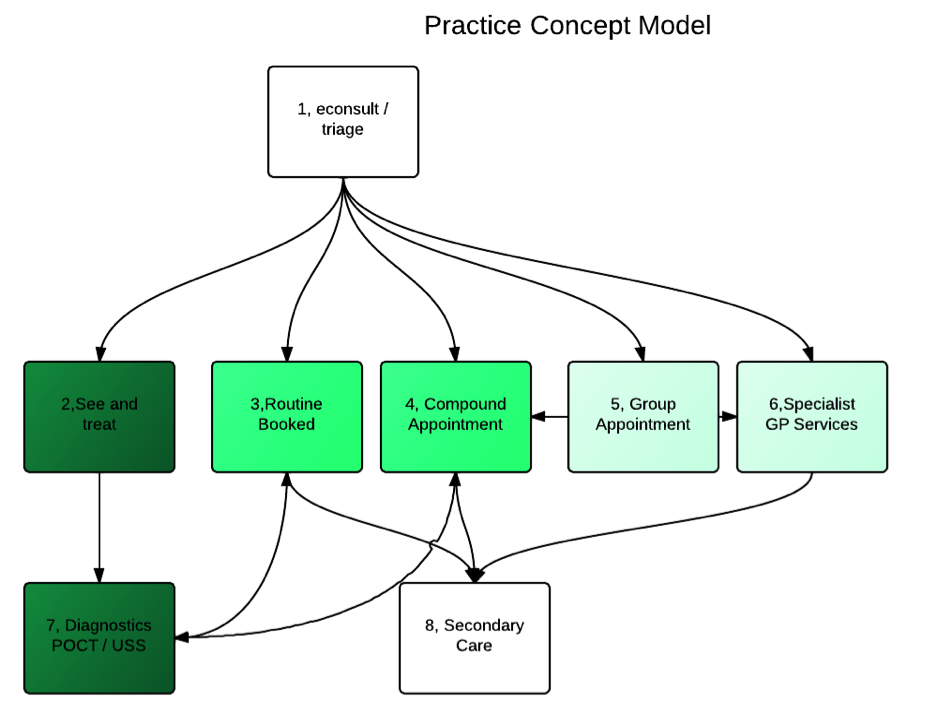
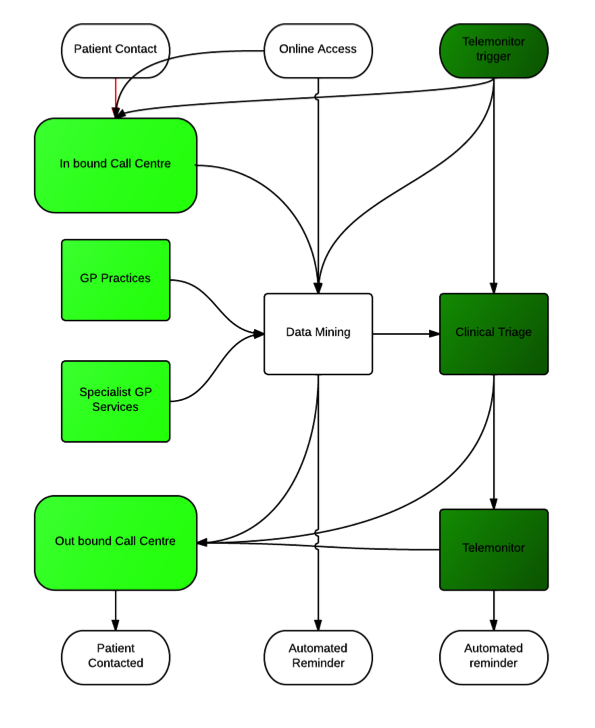
Access is sine qua non for primary care. Patients value access over continuity for urgent problems and continuity over access for non urgent or personal issues. However in deprived areas where need is greatest the dichotomy of access and continuity becomes skewed to access at the cost of long term conditions management.(Anwar et al., 2012) Similarly as demands increase receptionists are finding it harder to juggle the multiple pressures placed upon them without further training or changes in role.(Hammond et al., 2013). Since the turn of the century many practices across the world have been using the concept of advanced access (Murray and Berwick, 2003) (Longman, 2012) this seeks to address the patients problems in a “same day” way, not always through face to face consultation. Results have generally been favourable,(Salisbury et al., 2007) but the challenge to existing systems, ways of working and personal habits is significant and requires strong leadership. The KNMGP model proposes to deliver access through a centralised call centre approach. See Fig 1.
Although there is a long history of telephone consultations in primary care evidence is growing which identifies the pitfalls and possibilities for telephone consultations (Car and Sheikh, 2003)(McKinstry et al., 2009) In the KNMGP model we place triage and care navigation within the same functional space, although it should be noted that call handling may occur in a single location, the provision of triage and navigation should be considered as location independent. Appropriate members of staff who are working in practices will be called upon to provide triage and navigation as required, rather than expecting only staff based only in call centres to provide 100% of the function.
Telephony is not the sole method of patient contact, e-mail and web based services should also be implemented. Currently most GP system suppliers are in the process of developing apps/ portals to enable patients to book appointments directly, or access online booking/ test results/ prescription ordering. These are all taken as patient initiated contact.
Existing call management software, VOIP telephony and patient record can enable this distributed way of working.
Two other “access” methods exist alongside patient initiated contact. The call centre should use mined data to initiate contact with various patients or patient groups. This is distinct from telehealth which will be discussed later.
Fig 1 KNMGP Access concept.
The triage and navigation functions should be able to operate seamlessly from the patients perspective. Hand offs to other agencies may well be “cold” where data is passed but there is a delay involved in response to the patient, whereas transition from triage to navigation should be a “warm hand off” meaning the patient will have no delay in the proceedings.
Telephone based triage services have been received with mixed reviews, (McKinstry et al., 2009) especially when performed as in hours services, their use out of hours has been more openly received(Booker et al., 2013) and suggested as a means of demand management, care navigation and improved outcomes (Egbunike et al., 2010).
Electronic or online means of access often generate significant concerns in practitioners without experience of such methods, however published evidence suggests they have a role to play (Neville et al., 2004, p. -)
Intervention
Traditional models have a limited range of options at the disposal of triage services. Standard appointments, urgent appointments, occasionally telephone consults and less frequently non face to face interventions such as prescriptions issued without clinician/ patient contact.
The KNMGP model offers a wide range of options to the call centre and clinicians.
In most practices a small but significant proportion of patient management takes place without face to face contact. Medication reviews, appointment scheduling, resolution of scheduling issues and appointment can all occur without face to face clinical contact. However most diagnosis and intervention require clinician / patient contact, these interventions can occur as part of the call centre function, provided by clinicians based within practices, initial survey work at Wingate Medical Centre suggested 20% could be dealt with as non face to face or purely telephone consultations.
The call centre function clinicians and navigators have five in house opportunities which can be used for interventions. See and treat (2 in Fig 2 above) is essentially a walk in service, which dependant on local circumstances may be within the practice or alternate location. Routine booked appointment (3 above) is the familiar appointment system, however it should be flexible enough to offer variable length appointments as there is evidence to suggest this improves time usage and patient satisfaction (Sampson et al., 2013).
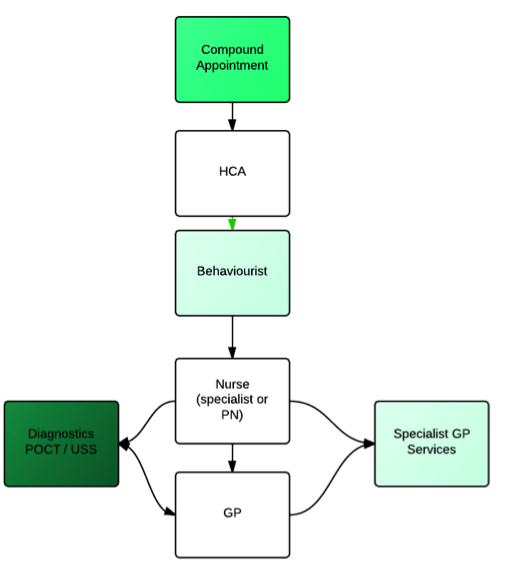
Patients with long term conditions often multi-morbid are becoming increasingly common (Smith et al., 2012a) and their management is challenging(Smith et al., 2012b) in single disease areas self care is becoming recognised as a useful tool (Taylor et al., 2012) whereas interventions such as exercise on prescription are struggling to make an impact(Pavey et al., 2011). We know that nurse led care is effective where good evidence exists but the flow experienced by the patient is often sub optimal (Stans et al., 2013) to correct this issue the KNMGP model proposes the use of compound consultations these are scheduled multidisciplinary consultations based on the Massachusetts General Hospital Ambulatory Practice of the Future model (Judge, 2005).
Although the functions within the compound consultation are noted as distinct tasks it is possible that they may be undertaken by various individuals dependant on skill set and patient needs.
A key change in the compound consultation is that the patient takes centre stage, remains in “their” room and the professionals undertake a “warm hand off” (Philibert, 2009) as required during the hour or so devoted to the patient in order that the patient participates in the transfer of information.
The HCA function is that of greeter and co-ordinator of the compound consultation. In addition the general demographic details and data associated with basic clinical care can be captured.
The Behaviourist function seeks to agree the patient’s life needs and aspirations, setting out their agenda for self care.
Many long term conditions are amenable to nurse led care packages (Fletcher and Dahl, 2013) including the supporting of self care (Taylor et al., 2012) the compound appointment beds the role of the nurse as a pivotal figure and for many patients the nurse may be the final step in the compound consultation. However it is envisioned that the Nurse function will be able to seek support from Point of care testing services or near patient diagnostics as well as specialist GP services (GPSI). It is possible that the scheduling of compound consultations may allow specialist nurses traditionally based in secondary care to become part of the primary care team when the needs of the patients require specialist intervention.
Point of care testing is still a relatively untested phenomenon (Al-Ansary et al., 2011) and further research is indicated to ensure its cost effectiveness, however, global trends in mobile technology and developments in laboratory services suggest that POCT will become a viable option in the lifetime of this model.
The GP function also has access to POCT and specialist services within the compound consultation. However the GP function remains the back stop for the patient with long term conditions, serving to resolve the issues generated when protocols are in conflict or medication outside of agreed protocol is required. It is anticipated that the time required for this function will be little different that currently involved in long term condition management, however the patient experience will be significantly changed.
Group Appointments are a proven intervention for engaging patients in the self care agenda,(Edelman et al., 2012)(Smith et al., 2012b), they can occur with a facilitator present ( more usually defined as Shared Medical Appointments ( SMAs)(Dickman et al., 2012)) or self facilitated.
enabling patients to use the central triage/ navigation function to arrange attendance at these appointments should facilitate their attendance.
Specialist GP Services cover a range of topics which may include access to GPs with specialist interest or services previously based in secondary care. GPSI functions are not universally distributed or accepted (Gérvas et al., 2007) and the evolution of primary care facing specialist services is still in progress (Bowling et al., 1997)(Beech et al., 2013) and as such this part of the model is clearly dependant on local variables. It is likely that access to specialist services will be via the traditional gatekeeper role, but facilitated by the triage/ navigation function.
Follow up
The KNMGP Model allows for a more systematic and multifaceted call and recall system than traditional practices. The model blends traditional patient generated requests for follow up “call me in a week” with online access to services and pivotally, telemonitor triggers (Seto et al., 2012). The data mining function is central to the practice model. Although initial data sources are likely to be in house data, captured from contacts in consultation, online service use and telemonitoring triggers there is huge potential for “big data” approaches (Murdoch and Detsky, 2013) to inform and assist in initiating call and recall. The field of data mining is still an emergent one(Marschollek et al., 2012)(Amini et al., 2013) but collation of data within an organisational footprint offers the use of tools such as PARR (Billings et al., 2012) to proactively schedule attention from physicians and telemonitoring services.
At this stage the architecture of the data mining element is uncertain. In the initial stages it may simply be a bank of regular searches producing a task list for contacts. As the technology evolves it is likely to become a proactive warning system based on real time intelligence.
Feasibility.
As referenced above the model has supporting evidence for each of its components. Many are at work in different parts of the NHS, but, to date, no single area has been able to combine the various components into a single model of primary care.
Currently primary care is under scrutiny for a model which has changed little since the inception of the NHS (Mathers, 2012) and both the Royal College of GPs and NHS England are completing major consultations on the future of General Practice (RCGP, 2012).
Initial cacluations within the LCD/TP organisation suggested that the model would be resource neutral given sufficient size and resource pooling to enable staffing and response issues to be met.
Within Wingate there has been an uncovering of significant levels of unmet need which mean this assumption is no longer likely to hold true. Further detailed modelling will be essential to validate the feasibility.
Source data
The UK general Practice workload survey 2006/7 (Information Centre, 2007).
Average patient list size of medical practitioners (excluding GP registrars and retainers) in general practice, by country, UK, 1964 - 2009 (Office of Health Economics, 2009)
Al-Ansary, L., Farmer, A., Hirst, J., Roberts, N., Glasziou, P., Perera, R., Price, C.P., 2011. Point-of-care testing for Hb A1c in the management of diabetes: a systematic review and metaanalysis. Clin. Chem. 57, 568–576.
Amini, L., Azarpazhouh, R., Farzadfar, M.T., Mousavi, S.A., Jazaieri, F., Khorvash, F., Norouzi, R., Toghianfar, N., 2013. Prediction and control of stroke by data mining. Int. J. Prev. Med. 4, S245–249.
Anwar, M.S., Baker, R., Walker, N., Mainous, A.G., 3rd, Bankart, M.J., 2012. Chronic disease detection and access: does access improve detection, or does detection make access more difficult? Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 62, e337–343.
Beech, R., Henderson, C., Ashby, S., Dickinson, A., Sheaff, R., Windle, K., Wistow, G., Knapp, M., 2013. Does integrated governance lead to integrated patient care? Findings from the innovation forum. Health Soc. Care Community.
Billings, J., Blunt, I., Steventon, A., Georghiou, T., Lewis, G., Bardsley, M., 2012. Development of a predictive model to identify inpatients at risk of re-admission within 30 days of discharge (PARR-30). Bmj Open 2.
Booker, M.J., Simmonds, R.L., Purdy, S., 2013. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emerg. Med. J. Emj.
Bowling, A., Stramer, K., Dickinson, E., Windsor, J., Bond, M., 1997. Evaluation of specialists’ outreach clinics in general practice in England: process and acceptability to patients, specialists, and general practitioners. J. Epidemiol. Community Health 51, 52–61.
Car, J., Sheikh, A., 2003. Telephone consultations. BMJ 326, 966–969.
Dickman, K., Pintz, C., Gold, K., Kivlahan, C., 2012. Behavior changes in patients with diabetes and hypertension after experiencing shared medical appointments. J. Am. Acad. Nurse Pract. 24, 43–51.
Edelman, D., McDuffie, J.R., Oddone, E., Gierisch, J.M., Nagi, A., Williams, J.W., 2012. Shared Medical Appointments for Chronic Medical Conditions: A Systematic Review, VA Evidence-based Synthesis Program Reports. Department of Veterans Affairs (US), Washington (DC).
Egbunike, J.N., Shaw, C., Porter, A., Button, L.A., Kinnersley, P., Hood, K., Bowden, S., Bale, S., Snooks, H., Edwards, A., 2010. Streamline triage and manage user expectations: lessons from a qualitative study of GP out-of-hours services. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 60, e83–97.
Fletcher, M.J., Dahl, B.H., 2013. Expanding nurse practice in COPD: is it key to providing high quality, effective and safe patient care? Prim. Care Respir. J. J. Gen. Pr. Airways Group 22, 230–233.
Gérvas, J., Starfield, B., Violán, C., Minué, S., 2007. GPs with special interests: unanswered questions. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 57, 912–917.
Hammond, J., Gravenhorst, K., Funnell, E., Beatty, S., Hibbert, D., Lamb, J., Burroughs, H., Kovandžić, M., Gabbay, M., Dowrick, C., Gask, L., Waheed, W., Chew-Graham, C.A., 2013. Slaying the dragon myth: an ethnographic study of receptionists in UK general practice. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 63, 177–184.
Information Centre, 2007. 2006/2007 UK General Practice Workload Survey.
Judge, D., 2005. Ambulatory Practice of the Future.
Longman, H., 2012. Access: The call we’ve all being waiting for. Health Serv. J. 122, 22–24.
Marschollek, M., Gövercin, M., Rust, S., Gietzelt, M., Schulze, M., Wolf, K.-H., Steinhagen-Thiessen, E., 2012. Mining geriatric assessment data for in-patient fall prediction models and high-risk subgroups. BMC Med. Inform. Decis. Mak. 12, 19.
Mathers, N., 2012. From cottage industry to post-industrial care? The RCGP response to the King’s Fund report on the quality of care in general practice. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 62, 326–328.
McKinstry, B., Watson, P., Pinnock, H., Heaney, D., Sheikh, A., 2009. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 59, e209–218.
Murdoch, T.B., Detsky, A.S., 2013. The inevitable application of big data to health care. Jama J. Am. Med. Assoc. 309, 1351–1352.
Murray, M., Berwick, D.M., 2003. Advanced access: reducing waiting and delays in primary care. Jama J. Am. Med. Assoc. 289, 1035–1040.
Neville, R., Marsden, W., McCowan, C., Pagliari, C., Mullen, H., Fannin, A., 2004. E-mail consultations in general practice. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 54, 546.
Office of Health Economics, 2009. Average patient list size of medical practitioners (excluding GP registrars and retainers) in general practice, by country, UK, 1964 - 2009.
Pavey, T.G., Taylor, A.H., Fox, K.R., Hillsdon, M., Anokye, N., Campbell, J.L., Foster, C., Green, C., Moxham, T., Mutrie, N., Searle, J., Trueman, P., Taylor, R.S., 2011. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. BMJ 343, d6462.
Philibert, I., 2009. Use of strategies from high-reliability organisations to the patient hand-off by resident physicians: practical implications. Qual. Saf. Health Care 18, 261–266.
RCGP, 2012. General Practice 2022 [WWW Document]. URL http://www.rcgp.org.uk/policy/rcgp-policy-areas/general-practice-2022.aspx
Salisbury, C., Goodall, S., Montgomery, A.A., Pickin, D.M., Edwards, S., Sampson, F., Simons, L., Lattimer, V., 2007. Does Advanced Access improve access to primary health care? Questionnaire survey of patients. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 57, 615–621.
Sampson, R., O’Rourke, J., Hendry, R., Heaney, D., Holden, S., Thain, A., Macvicar, R., 2013. Sharing control of appointment length with patients in general practice: a qualitative study. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 63, 185–191.
Seto, E., Leonard, K.J., Cafazzo, J.A., Barnsley, J., Masino, C., Ross, H.J., 2012. Mobile phone-based telemonitoring for heart failure management: a randomized controlled trial. J. Med. Internet Res. 14, e31.
Smith, S.M., Soubhi, H., Fortin, M., Hudon, C., O’Dowd, T., 2012a. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 345, e5205.
Smith, S.M., Soubhi, H., Fortin, M., Hudon, C., O’Dowd, T., 2012b. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst. Rev. Online 4, CD006560.
Stans, S.E., Stevens, J.A., Beurskens, A.J., 2013. Interprofessional practice in primary care: development of a tailored process model. J. Multidiscip. Healthc. 6, 139–147.
Taylor, S.J.C., Sohanpal, R., Bremner, S.A., Devine, A., McDaid, D., Fernández, J.-L., Griffiths, C.J., Eldridge, S., 2012. Self-management support for moderate-to-severe chronic obstructive pulmonary disease: a pilot randomised controlled trial. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 62, e687–695.