Follow up
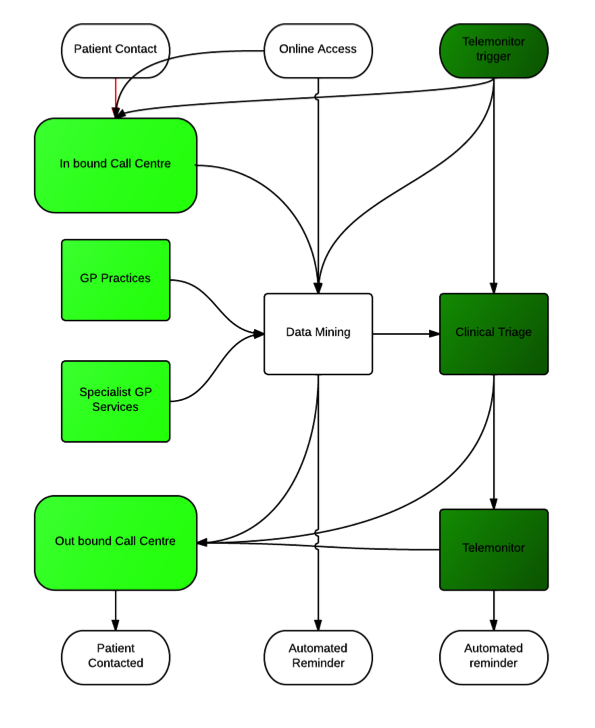
The KNMGP Model allows for a more systematic and multifaceted call and recall system than traditional practices. The model blends traditional patient generated requests for follow up “call me in a week” with online access to services and pivotally, telemonitor triggers (Seto et al., 2012). The data mining function is central to the practice model. Although initial data sources are likely to be in house data, captured from contacts in consultation, online service use and telemonitoring triggers there is huge potential for “big data” approaches (Murdoch and Detsky, 2013) to inform and assist in initiating call and recall. The field of data mining is still an emergent one(Marschollek et al., 2012)(Amini et al., 2013) but collation of data within an organisational footprint offers the use of tools such as PARR (Billings et al., 2012) to proactively schedule attention from physicians and telemonitoring services.
At this stage the architecture of the data mining element is uncertain. In the initial stages it may simply be a bank of regular searches producing a task list for contacts. As the technology evolves it is likely to become a proactive warning system based on real time intelligence.
Feasibility.
As referenced above the model has supporting evidence for each of its components. Many are at work in different parts of the NHS, but, to date, no single area has been able to combine the various components into a single model of primary care.
Currently primary care is under scrutiny for a model which has changed little since the inception of the NHS (Mathers, 2012) and both the Royal College of GPs and NHS England are completing major consultations on the future of General Practice (RCGP, 2012).
Initial cacluations within the LCD/TP organisation suggested that the model would be resource neutral given sufficient size and resource pooling to enable staffing and response issues to be met.
Within Wingate there has been an uncovering of significant levels of unmet need which mean this assumption is no longer likely to hold true. Further detailed modelling will be essential to validate the feasibility.
Source data
The UK general Practice workload survey 2006/7 (Information Centre, 2007).
Average patient list size of medical practitioners (excluding GP registrars and retainers) in general practice, by country, UK, 1964 - 2009 (Office of Health Economics, 2009)
Al-Ansary, L., Farmer, A., Hirst, J., Roberts, N., Glasziou, P., Perera, R., Price, C.P., 2011. Point-of-care testing for Hb A1c in the management of diabetes: a systematic review and metaanalysis. Clin. Chem. 57, 568–576.
Amini, L., Azarpazhouh, R., Farzadfar, M.T., Mousavi, S.A., Jazaieri, F., Khorvash, F., Norouzi, R., Toghianfar, N., 2013. Prediction and control of stroke by data mining. Int. J. Prev. Med. 4, S245–249.
Anwar, M.S., Baker, R., Walker, N., Mainous, A.G., 3rd, Bankart, M.J., 2012. Chronic disease detection and access: does access improve detection, or does detection make access more difficult? Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 62, e337–343.
Beech, R., Henderson, C., Ashby, S., Dickinson, A., Sheaff, R., Windle, K., Wistow, G., Knapp, M., 2013. Does integrated governance lead to integrated patient care? Findings from the innovation forum. Health Soc. Care Community.
Billings, J., Blunt, I., Steventon, A., Georghiou, T., Lewis, G., Bardsley, M., 2012. Development of a predictive model to identify inpatients at risk of re-admission within 30 days of discharge (PARR-30). Bmj Open 2.
Booker, M.J., Simmonds, R.L., Purdy, S., 2013. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emerg. Med. J. Emj.
Bowling, A., Stramer, K., Dickinson, E., Windsor, J., Bond, M., 1997. Evaluation of specialists’ outreach clinics in general practice in England: process and acceptability to patients, specialists, and general practitioners. J. Epidemiol. Community Health 51, 52–61.
Car, J., Sheikh, A., 2003. Telephone consultations. BMJ 326, 966–969.
Dickman, K., Pintz, C., Gold, K., Kivlahan, C., 2012. Behavior changes in patients with diabetes and hypertension after experiencing shared medical appointments. J. Am. Acad. Nurse Pract. 24, 43–51.
Edelman, D., McDuffie, J.R., Oddone, E., Gierisch, J.M., Nagi, A., Williams, J.W., 2012. Shared Medical Appointments for Chronic Medical Conditions: A Systematic Review, VA Evidence-based Synthesis Program Reports. Department of Veterans Affairs (US), Washington (DC).
Egbunike, J.N., Shaw, C., Porter, A., Button, L.A., Kinnersley, P., Hood, K., Bowden, S., Bale, S., Snooks, H., Edwards, A., 2010. Streamline triage and manage user expectations: lessons from a qualitative study of GP out-of-hours services. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 60, e83–97.
Fletcher, M.J., Dahl, B.H., 2013. Expanding nurse practice in COPD: is it key to providing high quality, effective and safe patient care? Prim. Care Respir. J. J. Gen. Pr. Airways Group 22, 230–233.
Gérvas, J., Starfield, B., Violán, C., Minué, S., 2007. GPs with special interests: unanswered questions. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 57, 912–917.
Hammond, J., Gravenhorst, K., Funnell, E., Beatty, S., Hibbert, D., Lamb, J., Burroughs, H., Kovandžić, M., Gabbay, M., Dowrick, C., Gask, L., Waheed, W., Chew-Graham, C.A., 2013. Slaying the dragon myth: an ethnographic study of receptionists in UK general practice. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 63, 177–184.
Information Centre, 2007. 2006/2007 UK General Practice Workload Survey.
Judge, D., 2005. Ambulatory Practice of the Future.
Longman, H., 2012. Access: The call we’ve all being waiting for. Health Serv. J. 122, 22–24.
Marschollek, M., Gövercin, M., Rust, S., Gietzelt, M., Schulze, M., Wolf, K.-H., Steinhagen-Thiessen, E., 2012. Mining geriatric assessment data for in-patient fall prediction models and high-risk subgroups. BMC Med. Inform. Decis. Mak. 12, 19.
Mathers, N., 2012. From cottage industry to post-industrial care? The RCGP response to the King’s Fund report on the quality of care in general practice. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 62, 326–328.
McKinstry, B., Watson, P., Pinnock, H., Heaney, D., Sheikh, A., 2009. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 59, e209–218.
Murdoch, T.B., Detsky, A.S., 2013. The inevitable application of big data to health care. Jama J. Am. Med. Assoc. 309, 1351–1352.
Murray, M., Berwick, D.M., 2003. Advanced access: reducing waiting and delays in primary care. Jama J. Am. Med. Assoc. 289, 1035–1040.
Neville, R., Marsden, W., McCowan, C., Pagliari, C., Mullen, H., Fannin, A., 2004. E-mail consultations in general practice. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 54, 546.
Office of Health Economics, 2009. Average patient list size of medical practitioners (excluding GP registrars and retainers) in general practice, by country, UK, 1964 - 2009.
Pavey, T.G., Taylor, A.H., Fox, K.R., Hillsdon, M., Anokye, N., Campbell, J.L., Foster, C., Green, C., Moxham, T., Mutrie, N., Searle, J., Trueman, P., Taylor, R.S., 2011. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. BMJ 343, d6462.
Philibert, I., 2009. Use of strategies from high-reliability organisations to the patient hand-off by resident physicians: practical implications. Qual. Saf. Health Care 18, 261–266.
RCGP, 2012. General Practice 2022 [WWW Document]. URL http://www.rcgp.org.uk/policy/rcgp-policy-areas/general-practice-2022.aspx
Salisbury, C., Goodall, S., Montgomery, A.A., Pickin, D.M., Edwards, S., Sampson, F., Simons, L., Lattimer, V., 2007. Does Advanced Access improve access to primary health care? Questionnaire survey of patients. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 57, 615–621.
Sampson, R., O’Rourke, J., Hendry, R., Heaney, D., Holden, S., Thain, A., Macvicar, R., 2013. Sharing control of appointment length with patients in general practice: a qualitative study. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 63, 185–191.
Seto, E., Leonard, K.J., Cafazzo, J.A., Barnsley, J., Masino, C., Ross, H.J., 2012. Mobile phone-based telemonitoring for heart failure management: a randomized controlled trial. J. Med. Internet Res. 14, e31.
Smith, S.M., Soubhi, H., Fortin, M., Hudon, C., O’Dowd, T., 2012a. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 345, e5205.
Smith, S.M., Soubhi, H., Fortin, M., Hudon, C., O’Dowd, T., 2012b. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst. Rev. Online 4, CD006560.
Stans, S.E., Stevens, J.A., Beurskens, A.J., 2013. Interprofessional practice in primary care: development of a tailored process model. J. Multidiscip. Healthc. 6, 139–147.
Taylor, S.J.C., Sohanpal, R., Bremner, S.A., Devine, A., McDaid, D., Fernández, J.-L., Griffiths, C.J., Eldridge, S., 2012. Self-management support for moderate-to-severe chronic obstructive pulmonary disease: a pilot randomised controlled trial. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 62, e687–695.